The video above features a lecture by health consultant and author Denise Minger at the 2016 Icelandic Health Symposium. Her 2014 book, “Death by Food Pyramid,” explores the roots of our beliefs about food and provides readers with tools to navigate conflicting dietary claims, and she does so in this lecture as well.
While Minger’s presentation primarily challenges our beliefs about low-fat diets, more broadly she also encourages everyone to keep an open mind, to question everything, to avoid group-think and premature assumptions based on the illusion of consensus. This is good advice for all of us.
As you may have noticed, I’ve made several U-turns myself over the years, as I delved deeper into various metabolic issues and gained a deeper understanding about how the human body works.
Optimal health is not a one-and-done, but rather an ongoing journey. New information surfaces. Your body changes with age, and new environmental factors come into play. So, we must adapt to changing circumstances and learn to listen to our bodies.
For many years, I was convinced a long-term, high-fat diet was the way to go, and that fat burned “cleaner” than glucose. I’m now coming to understand that there’s far more to this equation than I had previously appreciated, and that carbs, fructose in particular, have been wrongly blamed for damage that actually isn’t the fault of sugar itself.
I’m presenting Minger’s lecture here as food for thought. It’s not a wholesale endorsement of her views, but an opportunity to hear the other side of the high-fat/low-fat argument.
As noted by Minger, the history we’re told is not necessarily the whole truth. It’s typically curated to create a particular narrative, and this applies to the history of dietary recommendations as well. I think you’ll really enjoy it, as she presents a rather revolutionary hypothesis that, indeed, may clear up much of the confusion surrounding high- versus low-fat.
The Prevailing History of Low-Fat Diets
Minger starts out by reviewing the history of low-fat diets because, according to her, this is where most get off track. Physiologist Ancel Keys — creator of Army K rations — is typically credited with starting the low-fat movement in the 1950s.1
According to the prevailing narrative, he cherry picked data to show that the more saturated fat a population ate, the higher the rate of heart disease. He then used his charisma and influence to convince the American Heart Association to adopt low-fat dietary guidelines and promote that for cardiovascular health.
The first “Dietary Goals for the United States” were published in 1977 by the U.S. Senate Select Committee on Nutrition and Human Needs, chaired by Sen. George McGovern.2 This report eventually grew into what today is known as the U.S. Dietary Guidelines.
For the first time, the government was making recommendations about what to eat to maintain good health, and they specifically recommended that people increase consumption of carbohydrates and reduce saturated fat intake.
However, as the low-fat recommendation took hold, obesity skyrocketed. The subsequent obesity epidemic has long been viewed as evidence that the low-fat recommendation was in error.
Did Low-Fat Diets Cause the Obesity Epidemic?
But not so fast, Minger says. While low-fat diets were in fact pushed, did Americans really follow that recommendation? Looking at macronutrient intake data, Minger points out that while Americans did raise their carb intake after the guidelines were released, they did not cut their fat intake. Portion sizes also went up, and sugary snacks were coming onto the scene.
Interestingly, though, if you look at macronutrient intake data from the early 1900s, carb intake (in terms of grams per day) at that time was quite similar to what it was in 2000.
“So, we can’t really even say that our diet was higher carb than it has ever been,” she says. “Not only that, but things look very interesting on a global level when we consider what other countries are eating.
We can see that as the percent of total calories, America actually has a very, very low, relatively speaking, intake of carbohydrate compared to a lot of other countries.
Other countries with low carbohydrate intakes, relatively speaking, include Australia, Iceland, a lot of different parts of Europe, many places that are also experiencing obesity epidemics.
And if we look at relative fat intake, we can see that America, Australia, Europe, Iceland — again many of the same areas experiencing obesity epidemics — actually have the highest intake of fat. So, bottom line here is that you do not eat a low-fat diet in the West at all. We can’t really blame anything that’s going on, on … low-fat [diets].”
The Forgotten Timeline of the Low-Fat Movement: Dr. Kempner
Menger goes on to review how, in 1939, Walter Kempner, a medical doctor and research scientist, used low-fat diets to successfully treat a wide array of chronic disease, including kidney disease and kidney failure, high blood pressure, diabetes, heart disease, psoriasis and more.
He’s been referred to as the father of modern diet therapy, and is the creator of the Rice Diet, which was based on 250 grams to 350 grams of white rice (dry weight), unlimited fresh fruit and fruit juice, and, shockingly, unlimited white sugar. On average, his patients consumed between 100 grams to 400 grams of refined sugar a day. This diet is basically 94% carbs and only 2% fat.
The result? Patients with a range of diseases (listed above) dramatically improved, including diabetics. In a study that followed patients for up to 11 years, Kempner found that only 15% of diabetics experienced a rise in fasting blood sugar on the Rice Diet; 22% had no change; and 63% experienced a decrease, with an average drop of 101 mg/dL.
Insulin usage also decreased by 58% and 1 in 4 were able to cease taking insulin because their levels were completely normalized. A quote from a conference paper reviewing the Rice Diet reads:3
“Patients … were able to transition into a more flexible diet over time, while leading a normal, active life, without medications, indicating that the disease state [i.e., diabetes] had been permanently modified.”
The Forgotten Timeline: Drs. Morrison and Swank
In the 1940s, Dr. Lester Morrison, another pioneer of the low-fat diet, used a low-fat diet to treat heart disease in people who had already experienced a heart attack. The “Morrison Diet-Heart Study,”4 begun in 1946, found that people in the low-fat diet group had about half the mortality rate of controls after three years (14% compared to 30%).
Fat was the only macronutrient that was limited. The test group maintained daily fat intake between 20 grams and 25 grams, while eating as much sugar and refined grains as they wanted. After eight years, the low-fat group still had a lower mortality rate — 44% — compared to controls at 76%.
In the late 1940s, Dr. Roy Swank was a neurologist who not only advocated a low-fat diet, but also treated multiple sclerosis (MS) patients with it.5 He developed a theory that MS was the result of genetics combined with dietary triggers, saturated fat in particular. He put 150 MS patients on a low-fat diet (max 10 grams to 15 grams of saturated fat a day, primarily from meat and dairy). Sugar and refined grains were not limited.
Swank followed his patients for up to 50 years. Follow-up after 34 years showed that disease progression stabilized among those who adhered to the low-fat recommendation, while worsening among those who went back to eating more fat.
Mortality statistics confirmed this, showing that 31% of those who had died during the 34th year of follow-up had been eating less than 20 grams of saturated fat a day, while 80% of those who had died had been eating more than 20 grams.
The Forgotten Timeline: Drs. Pritikin and Esselstyn
Keys doesn’t enter the low-fat scene until the mid-1950s. By then, doctors had already been using low-fat diets in clinical practice for decades, with good success.
“So, Ancel Keys is not really the beginning of the low-fat movement,” Minger says. “There are a few people who have been swept under the rug of history, whom we’ve forgotten about.”
In the late 1950s, Dr. Nathan Pritikin founded a longevity center and became well-known for treating obesity and heart disease with a very low-fat diet based on vegetables, grains and fruits.
Then, in 1977, the first U.S. dietary guidelines recommending low fat came out. So, these guidelines were not necessarily the result of Keys’ alleged charisma, but did in fact have a long history of clinical successes to back them up.
Minger also reviews more recent research by Dr. Caldwell Esselstyn, a cardiac surgeon who in 2014 published the results of a five-year study using an extremely low-fat, plant-based diet on 198 patients with advanced heart disease. Of those, 177 adhered to Esselstyn’s strict diet. The rest ended up serving as an accidental control group.
Among adherents, 22% completely reversed their heart disease, and only one person — 0.6% — had a cardiac event (stroke), compared to 62% of nonadherents.
“So, can we really say that low-fat, high-carb diets categorically are bad for cardiovascular health when … very, very, very low-fat [diets] have been shown —with evidence in clinical settings — to reverse heart disease? We need to refine the way we’re looking at these things,” Minger says.
Why Don’t Low-Fat Diets Work Today?
All of this brings us to an important question. If low-fat diets were so effective in decades past, why don’t they work today? Most modern research suggests low fat isn’t effective. The answer, Minger says, is that we’ve redefined the term “low fat.”
Between 1930 and 1970, “low fat” meant fat accounted for 10% of calories or less. Since the 1980s, “low fat” has been redefined as 30% of calories, which by all accounts is more like “moderate fat,” or even “relatively high fat,” based on the average global fat consumption. Minger then presents a rather intriguing, if not revolutionary, hypothesis.
We know that when your diet is 65% or more fat, you enter a metabolic state called ketosis, which has a long list of health benefits. “What if,” Minger says, “on the other end of the spectrum there’s a mirror metabolic state that happens when you restrict fat to [10% or less]?” The image below, from her slide show, illustrates her novel hypothesis.
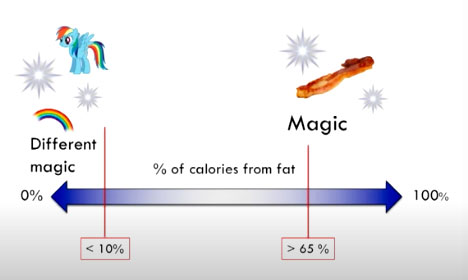
Minger has dubbed this low-fat metabolic state “carbosis,” because there’s no official name for it. She explains:
“We got ketosis on one end; we got carbosis on the other end, and my thought is that what’s in the middle is the macronutrient ‘swamp land.’ And this swamp land, unfortunately, is where most of our obesity-producing diets tend to fall.
We see that a toxic combination [of] very processed carbohydrates with industrial vegetable oils … mixed with some salt, become highly addictive, maybe cause some changes in appetite regulation …
But the important thing here is … we have USDA guidelines that fall here, American Heart Association guidelines that fall here, American Diabetes Association guidelines that fall here, American Dietetic Association guidelines that fall here.
And, most importantly, if you look at almost any ‘low-fat’ study that has been conducted in recent years, it is also going to use a fat intake of about 30% — swampland values.
Of course, it’s not going to [produce] that therapeutic effect that we saw in some of this older research. That also brings us to a new question, which is why does [fat] need to be so low in order for that magic to happen?”
Dietary Fat Reduces Insulin Sensitivity
Minger goes on to review evidence suggesting that fat can reduce insulin sensitivity. Importantly, many experiments try to extrapolate the effects of macronutrients based on processed foods loaded with unnatural ingredients like hydrogenated soybean oil. That’s not a reliable way to ascertain the effects of fats and carbs found in whole foods.
One study, however, used just two basic ingredients: potato and butter. Metabolically healthy, nondiabetic, lean adults were fed a baked potato (50 grams of carbohydrate) either alone, or with 50 grams of butter. There’s a belief that eating fat with a high-carbohydrate meal will result in a lower blood sugar spike and insulin response, and this is what they wanted to test.
“As predicted, adding the fat to the potato did lower the glucose response, but it did not dramatically, significantly lower the insulin response. In fact, adding fat to the potato caused insulin levels to stay elevated for an hour longer than eating the potato alone.
It took a longer time for that level to return to baseline … and there was actually a potentiating effect on insulin from the fat. What that means is, more insulin was needed to handle the same amount of blood sugar when fat was added to the potato … So, for some reason the insulin was not being as effective, or it was circulating abnormally …”
They then repeated the experiment using patients with untreated Type 2 diabetes. They ate either a baked potato alone, or with varying amounts of fat from butter, ranging from 5 grams to 50 grams.
Interestingly, in diabetics, adding fat did not lower the blood sugar response. The insulin response to potato alone was also lower than it was for potato with as little as 5 grams of fat. The effect leveled off at 15 grams of fat, but all insulin responses were higher with fat than with potato alone.
“So, there’s something about adding butter to a high carbohydrate meal that increases insulin levels relative to the carb food being eaten alone,” Minger says.
This could explain why the Rice Diet, which was 94% carbohydrate and only 2% fat, improved insulin levels in diabetics. Kempner himself observed that even minimal additions of fat spoiled the therapeutic effect.
Dietary Fat Reduces Blood Oxygen
There’s also evidence suggesting that dietary fat can reduce the ability of oxygen to reach different tissues, including your brain and heart. Minger cites a 1955 study in which 14 patients with angina (a form of heart disease that causes severe chest pain) fasted overnight and were then given a glass of heavy cream to drink the next morning.
They then measured the plasma lactescence,6 a marker for fat flooding the blood stream during the process of digestion. Plasma lactescence started rising after two hours of ingestion, peaking at Hour 3. And, right as plasma lactescence peaked, that’s when patients began to experience bouts of angina and abnormal EKGs.
There were 14 angina attacks among the 14 patients, but some experienced multiple attacks while others had none. During peak lactescence, there was also a reduction in oxygen carrying capacity, meaning less oxygen was reaching their hearts. On top of that, platelets and red blood cells started clumping together, so blood flow was impaired.
They then replicated the experiment using an isolated protein powder drink with dextrin and maltose that had the same calorie content as the heavy cream. And, while this drink objectively contains less healthy ingredients, after five hours, none of the patients had experienced an angina attack and none had abnormal EKG.
“So, something to think about: There might be … certain susceptibilities among certain people to be sensitive to a high saturated fat intake,” Minger says.
“I’m not going to draw conclusions right now. This is still something I’m researching. But for anybody who does have any type of heart condition, consuming a lot of saturated fat in one meal might not be the best idea.”
Conclusion
In conclusion, Minger notes:
“… we sometimes blame carbohydrates for breaking our carbohydrate metabolism … We have another option though … This is what I’m thinking: Low carbohydrate diets are amazing for managing the symptoms and expressions of insulin resistance.
If you’re diabetic, you can go on a low carbohydrate diet, normalize your blood sugar, normalize your a1c, do great on the Surface, but if you ever go back to eating carbohydrates, you will be in trouble. There is still something about the body that is broken …
For some people, [their] bodies may be permanently broken beyond repair. I’ll definitely acknowledge that. But for some people, there may be the potential to actually restore glucose control … restore metabolic flexibility, and actually heal things like diabetes.
And right now, there is more evidence that a very low-fat diet can do that than a very high fat diet can … So, it’s a matter of, what are we willing to risk? What are we willing to play around with? …
So, I would like to leave with this one thought, which is that we have been engaged in a macronutrient war for a very, very long time — decades. The first victim was fat. We decided that was bad … [E]ventually we started realizing that that strategy didn’t work so well. Then we started targeting carbohydrates …
In my opinion this is also very narrow-minded. Both of these macronutrients operate in ways that are context-dependent. Fat can make carbohydrates look bad. Carbohydrates can make fat look bad. But in reality, we have these two different worlds that, most of the time, we consider irreconcilable, mutually exclusive.
We can’t figure out why one would work and the other one would work. So we tend to choose sides and root for just one. I would like to offer the idea that maybe these two things are not in fact at odds.”
