A Year into our collective coronavirus experience, Americans remain stressed, with physical health taking a back seat to our daily grinds based on the 2021 Stress in America survey from the American Psychological Association (APA).
The APA has been updating us on U.S.-stress for several years, and more frequently since the start of the COVID-19 pandemic at the start of 2020.
In their latest report, APA updates their previous profiles of Americans’ stress looking into different demographic groups and coping mechanisms.
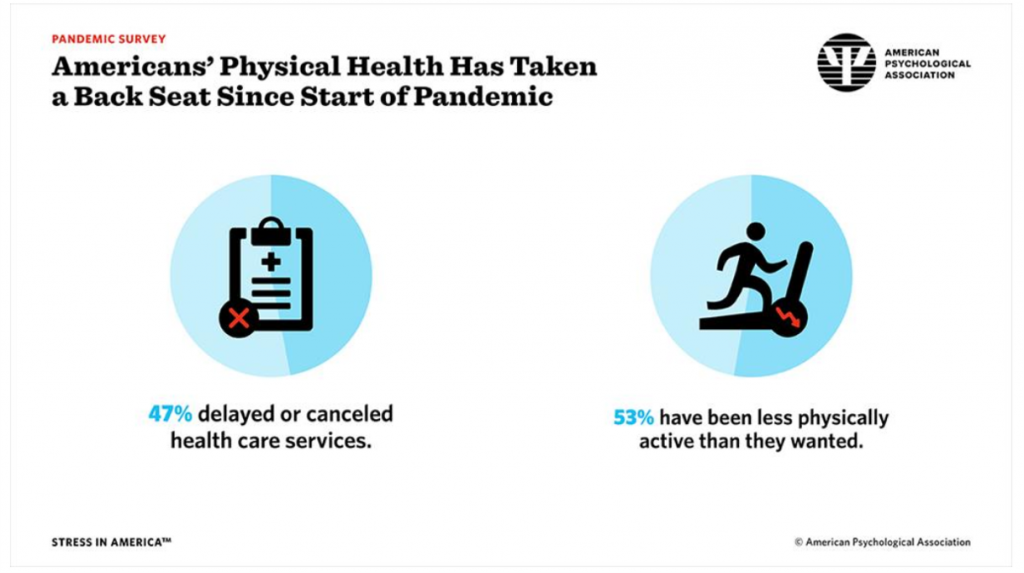
The topline, across all adults living in America, is that one-half have delayed or cancelled health care services. One-half has also been less physically active than they had ideally wanted.
The APA polled 3,013 U.S. adults 18 and older in February 2021. The survey sampled a sufficient number of essential workers to ensure statistical significance for that group’s responses, along with balancing parental status, age of children, and race/ethnicity of the respondents.
 Beneath those two macro-statistics on personal health — opting out of medical care services and being less physically active — most Americans had undesired weight changes, with 42% saying they gained more weight than they intended to. For those people, the average weight gain was 29 pounds, with a median of 15 pounds.
Beneath those two macro-statistics on personal health — opting out of medical care services and being less physically active — most Americans had undesired weight changes, with 42% saying they gained more weight than they intended to. For those people, the average weight gain was 29 pounds, with a median of 15 pounds.
Sleep has also been interrupted for two in three Americans, some sleeping more than they want, and some getting much less sleep than desired. This concept of “corona-somnia” is getting a lot of media attention, and especially today being World Sleep Day is in the headlines in mass media. It is yet another side-effect of the COVID-19 pandemic and accompanying anxiety.
For some working Americans, the stress has led to diagnoses of mental health disorders — especially acute among essential workers, shown in the second graphic from the report. Three in four essential workers said they could have used more emotional support than received.
 The APA also looked closely at U.S. parents’ level of anxiety and stress and subsequent impacts on physical and mental health. One in four parents was diagnosed with a mental health disorder since the emergence of the COVID-19 pandemic.
The APA also looked closely at U.S. parents’ level of anxiety and stress and subsequent impacts on physical and mental health. One in four parents was diagnosed with a mental health disorder since the emergence of the COVID-19 pandemic.
Mothers’ mental health worsened compared with fathers’ based on the APA research, with fathers more likely to report resultant behavioral and physical health impacts.
One-half of parents said stress in their life increased after the pandemic. While one-in-three parents reported getting treatment from a mental health professional during the pandemic, three-quarters of parents said they could have used more emotional support than they received.
Nearly one-half of Dads reported drinking more alcohol to cope with stress in the pandemic, and 29% of Moms were drinking more.
 Health Populi’s Hot Points: In today’s Hot Points, I want to pull out this large and detailed data chart on Black Americans’ views on the future. We well understand the disproportionate impact that the coronavirus has exacted on Black and Hispanic Americans in the past year.
Health Populi’s Hot Points: In today’s Hot Points, I want to pull out this large and detailed data chart on Black Americans’ views on the future. We well understand the disproportionate impact that the coronavirus has exacted on Black and Hispanic Americans in the past year.
The APA conducted an additional study in the weeks following the death/murder of George Floyd last summer, which I discussed here in Health Populi.
In that study conducted in June 2020, 55% of Black adults said discrimination was a significant source of stress — compared with 42% saying so in May, just one month earlier (before George Floyd’s demise).
This chart reflects Black Americans responses to two scenarios:
- My comfort in going back to living life like I used to before the pandemic and,
- My easy about adjusting to in-person interactions once the pandemic ends.
You can see from the red bars that more Black people in the U.S. are uncomfortable going back to living life “like I used to” pre-COVID, as well as more feeling uneasy adjusting to in-person interactions post-COVID.
Among the many health disparities the pandemic shined a light on were a few that converge, highly relevant to these scenarios:
We know that mental health will be a pandemic long-persisting past Americans’ achieving some level of herd immunity against the coronavirus. We also know that without attending to and breaking down peoples’ access to mental health services, physical health and other negative outcomes will exacerbate.
 As a just-breaking signal illustrating how the private sector can help address #mentalhealth and physical health at the same time, Whole Foods began collaborating with Headspace to bolster consumers’ well-being and mindful eating. This is a terrific example of the breaking down of siloes to help make health better for people. #FoodIsMedicine.
As a just-breaking signal illustrating how the private sector can help address #mentalhealth and physical health at the same time, Whole Foods began collaborating with Headspace to bolster consumers’ well-being and mindful eating. This is a terrific example of the breaking down of siloes to help make health better for people. #FoodIsMedicine.
Here are links to my previous posts on the APA Stress in America study…
Stress in America, Like COVID-19, Impacts All Americans
Stressed Out by COVID and Civil Unrest – the APA’s Stress in America Survey, Part 2
Stress in America – COVID-19 Takes a Toll on Finances, Education, Basic Needs and Parenting, Part 1
