Researchers at Duke University have developed a fluid dynamics simulator that can model blood flow within the body, including the motion of individual blood cells. The researchers hope that the system could eventually be used by clinicians to model blood flow for individual patients and help with treatment decisions, such as stent placement.
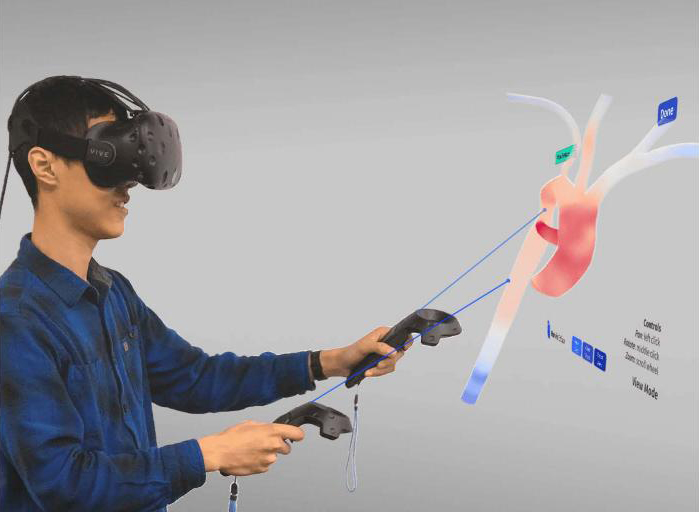
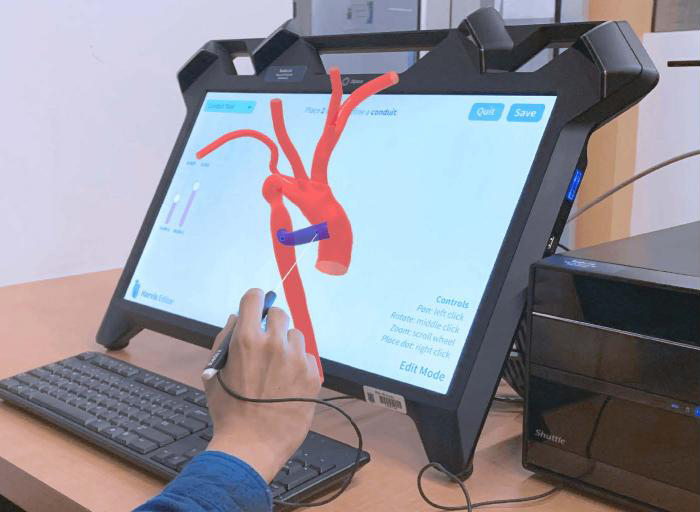
By testing various graphical user interfaces for the system, the research team learned that both a virtual reality system and a traditional computer were easily used by participants, but most preferred the VR interface, suggesting that it could help to increase user uptake of the system.
“As cardiovascular disease continues to be the number one cause of death in the US, the ability to improve treatment planning and outcome remains a significant challenge,” said Amanda Randles, a researcher involved in the study. “With the maturity and availability of VR/AR devices, we need to understand the role these technologies can play in the interaction with such data. This research is a much-needed step for developing future software to combat cardiovascular disease.”
The research team has been developing this software for over a decade. So far, they have shown that it can be used to model blood vessels from individual patients using data from biomedical imaging. Moreover, the system can also model blood flow through the entire body if required.
However, in its original form, the system wasn’t easy to use, requiring knowledge of computer programming languages, meaning that it wouldn’t be accessible to clinicians. To solve this, the researchers have been developing a graphical user interface, and have recently experimented with several methods with which users can interact with the 3D vascular models, including the traditional computer monitor and mouse approach and an immersive virtual reality approach.
They tested the interfaces by asking students and researchers to model cardiovascular procedures, such as stent placement, in the 3D simulation. The participants were able to use the different interfaces without too much difficulty, but enjoyed the VR headset the most.
“People enjoyed the 3D interface more,” said Randles. “And if they enjoyed it more, they’re more likely to actually use it. It could also be a fun and exciting way to get students engaged in classes about the vasculature system and hemodynamics.”
See a video about the system below:
Study in Journal of Computational Science: Harvis: an interactive virtual reality tool for hemodynamic modification and simulation
Via: Duke University
