In a laboratory in New York City, researchers coaxed a key piece of the coronavirus — its infamous outer “spike” — to mutate so that it became invisible to disease-fighting antibodies, according to a new study that has not yet been published in a scientific journal.
The provocative finding should not set off alarm bells, experts said. The altered spikes were not attached to the real coronavirus, which mutates at a much slower pace than most laboratory viruses. But the study does underscore the need for treatments and vaccines that attack the virus in different ways, so that if the pathogen manages to evade one approach, another will be waiting in the wings.
“It’s an old story for virology,” said Dr. Sallie Permar, a virologist and pediatrician at Duke University who was not involved in the study. “If you only target one little region, that virus is going to find a way to get away from it. It’s why viruses are so successful in this world.”
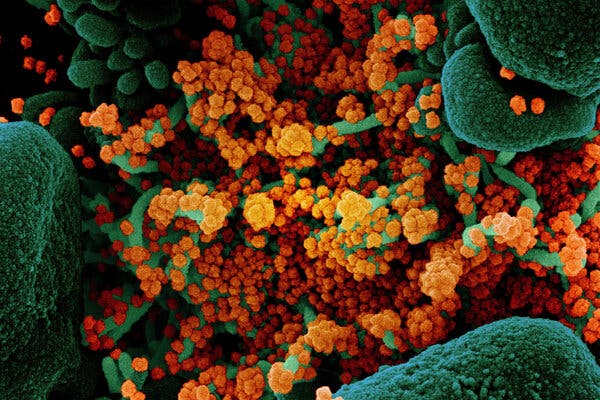
Many vaccines against the coronavirus, as well as several treatments, take aim at its spike protein, the virus’s most potent weapon — and its Achilles’ heel. Without its spikes, the pathogen can’t get into human cells.
Therapies based on this potent protein could stop infections in their tracks. Some promising vaccines, for example, prompt the body to make spike-specific antibodies that might vanquish the virus. And many companies in the race to find coronavirus treatments are making synthetic versions of these molecules, called monoclonal antibodies, to mimic this process en masse.
But all viruses are moving targets. When they replicate, their genetic material doesn’t copy itself perfectly, and mistakes are common. Although most of these mutations are inconsequential, they occasionally lead to noticeable changes in the viruses’ appearance — some of which may disguise them from the immune system. Cavalries of antibodies trained to recognize one version of spike might be totally discombobulated by another, leaving the person vulnerable to disease.
To study these key mutations, a team led by Rockefeller University virologists Theodora Hatziioannou and Paul Bieniasz created synthetic, fast-mutating viruses that carried the coronavirus spike. They then flooded the faux pathogens with different types of monoclonal antibodies known to glom onto the spike, and added healthy cells for the viruses to infect.
When exposed to the deluge of antibodies in the lab, a small proportion of viruses with modified spike proteins eluded the onslaught. Some even managed to replicate inside cells.
“These are the mutations that are potentially problematic,” Dr. Bieniasz said.
Some of these very same spike mutations are already circulating at very low levels among people, according to genetic sequences of the novel coronavirus collected from around the world. But this isn’t necessarily reason for concern, experts said. In most cases, the changes were found in less than 0.1 percent of the coronavirus sequences known so far. That still leaves “more than 99.9 percent of the sequenced viruses susceptible” to the antibodies tested in the study, said Nathan D. Grubaugh, a virologist at Yale University who was not involved in the study.
The study also suggests that coronaviruses with these anomalous spikes are no more prevalent than those with other genetic backgrounds, said Christopher Barnes, a structural biologist who is collaborating with the study team on new work. And real coronaviruses carry proofreading machinery that makes their replication process less error-prone.
“You can get these mutations,” Dr. Barnes said. “But I don’t think these mutations are going to be driving events that we have to worry about.”
In theory, concerning spike mutations could become more common if the coronavirus experiences pressures akin to the team’s synthetic virus in the lab — if hordes of people used the same monoclonal antibody therapy, for instance, then passed resistant pathogens to others. But even in that highly unlikely scenario, the virus could be thwarted with a combination of antibodies.
The coronavirus’s spike has an intricate architecture, full of nooks and crannies that different antibodies, each with its own preferred spot, can stick to. Mixing different types of antibodies together could form a phalanx around the virus from several angles at once.
Even if the virus was able to shirk one antibody’s grasp, “the chances that it evolves multiple mutations in one go is infinitesimal to none,” said Harry E. Taylor, a virologist and immunologist at SUNY Upstate Medical University who was not involved in the study. “That effectively corners the virus.”
That exact scenario played out when the researchers repeated their experiments, this time dosing the virus with two types of monoclonal antibodies instead of one. Some zeroed in on the part of the spike that directly contacts human cells, while others shackled a different piece of the protein. The virus could not fend off both assailants at once.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
Several types of monoclonal antibodies are now in clinical trials. If all goes well, such concoctions might not only treat coronavirus infections but also prevent them. That could help millions of people, especially as the world awaits a vaccine, said Akiko Iwasaki, an immunologist at Yale University who was not involved in the study.
Studies like these could help researchers identify ideal antibody targets on the spike, Dr. Taylor said. Some pieces of the protein, for instance, will never mutate successfully because they are essential to the virus’s ability to break into cells. That makes them easy prey for the immune system.
But the new findings also hint that single-antibody formulations “may not be as successful,” Dr. Taylor said, at least in the long term. Developing a cocktail containing a diverse blend of antibodies could be a safer bet.
Such mixtures would also more accurately mimic the body’s natural response to the coronavirus. In the study, viruses flushed with samples of convalescent plasma — fractions of blood donated by people who have recovered from Covid-19 — struggled to infect cells.
Some scientists, including those at American biotechnology company Regeneron, are already attempting this combo approach, mixing two potent types of monoclonal antibodies into a single treatment.
But Dr. Iwasaki pointed out that antibody cocktails might be tougher to bring to market. “Every time you make a drug, you get approval for each component separately,” she said. Even so, the data so far indicates that “you don’t need hundreds of monoclonals” to subdue this virus, she added. Two might be plenty.
The lesson of diversity might be even more powerful for vaccines, which can marshal a multifaceted immune response. Some immune cells and molecules will be tailored to home in on the spike, whereas others might prefer other parts of the virus. Vaccines that present the body with many pieces of the coronavirus, rather than the spike alone, could have a better shot at triggering a suite of these defenses, said Dr. Taia Wang, an immunologist at Stanford University who was not involved in the study.
As long as the coronavirus has people to infect, it will have opportunities to mutate, sometimes in ways that could bode poorly for us. But some informed forecasting is already helping scientists stay one step ahead, Dr. Permar said: “This is an excellent way to see into the future and figure out what we may need to be looking out for.”
