Advertisement
Supported by
Medical Journals Reluctant to Take On Racism, Critics Say
An editor’s departure at JAMA is bringing calls for a sharper focus on racism and its consequences.

The top editor of JAMA, the influential medical journal, stepped down on Tuesday amid a controversy over comments about racism made by a colleague on a journal podcast. But critics saw in the incident something more pernicious than a single misstep: a blindness to structural racism and the ways in which discrimination became embedded in medicine over generations.
“The biomedical literature just has not embraced racism as more than a topic of conversation, and hasn’t seen it as a construct that should help guide analytic work,” said Dr. Mary Bassett, professor of the practice of health and human rights at Harvard University. “But it’s not just JAMA — it’s all of them.”
The longstanding issue has gained renewed attention in part because of health care inequities laid bare by the pandemic, as well as the Black Lives Matter protests of the past year. Indeed, an informal New York Times review of five top medical journals found that all published more articles on race and structural racism last year than in previous years.
It was only in 2013 that racism was first introduced as a searchable keyword in PubMed, the government’s vast medical library. Since then, however, the five journals have published many more studies mentioning race than those mentioning racism. JAMA published the fewest studies mentioning racism, the review found.
‘Race’ and ‘Racism’ in Prominent Medical Journals
Five influential medical journals published more articles that included the word “racism” in 2020 than they had in previous years. Only JAMA still published more articles on race as a socioeconomic concept than those that addressed systemic racism.
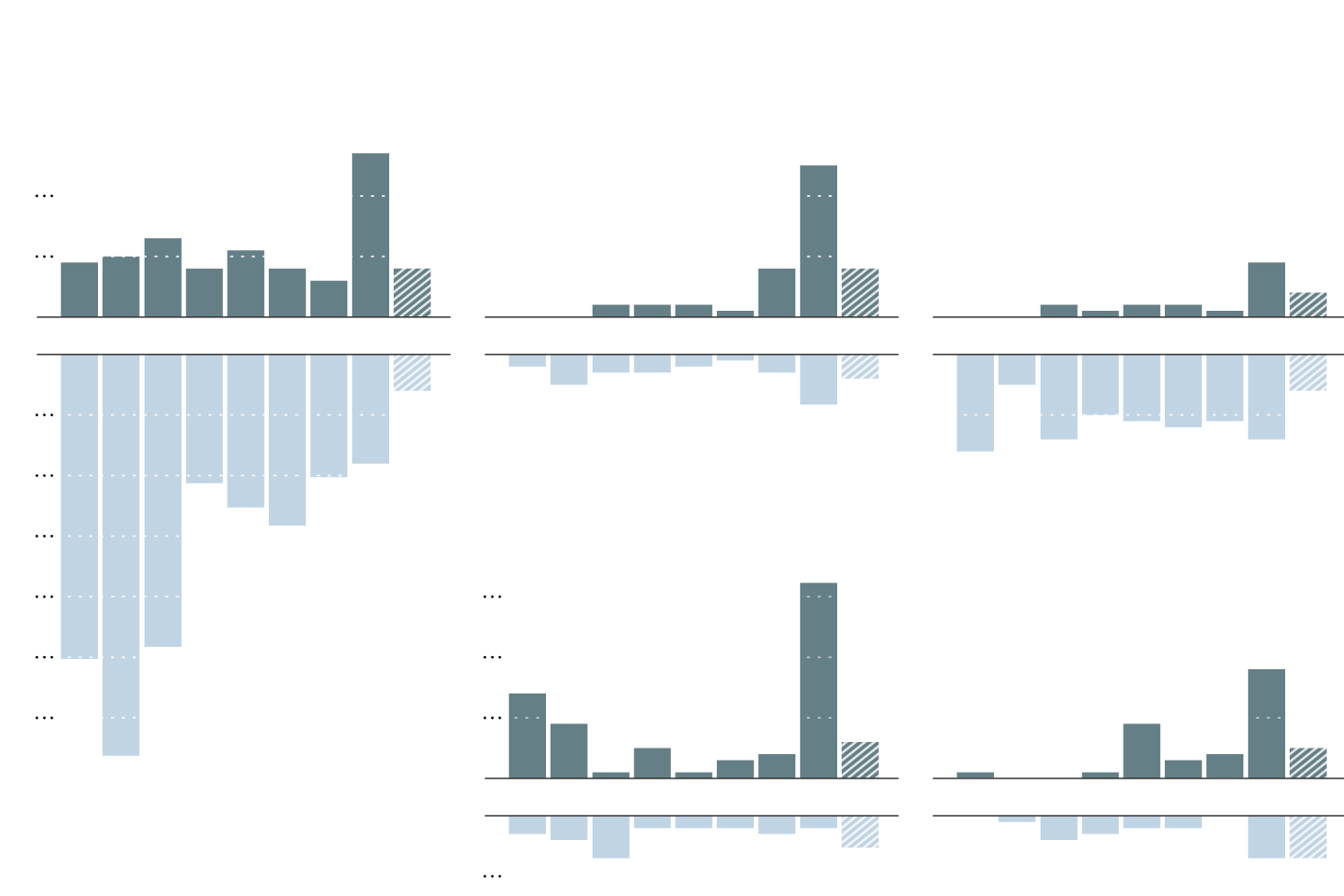
UNITED STATES
JAMA
American Journal
of Public Health
The New England
Journal of Medicine
Number of articles
in a PubMed search
for “racism”
20
10
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
10
20
BRITAIN
30
The BMJ
The Lancet
In a PubMed
search for
“race”
40
30
50
20
60
10
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
10
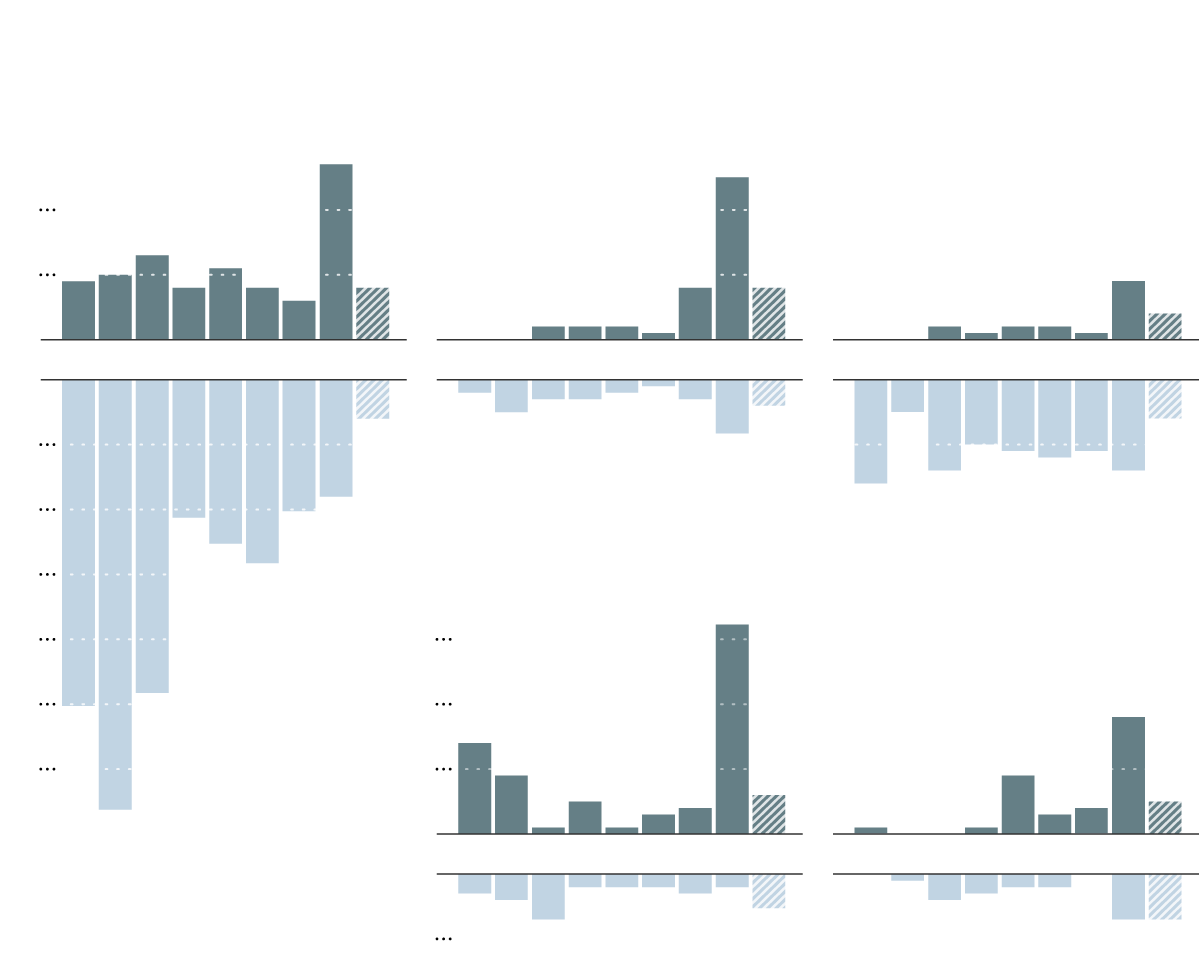
UNITED STATES
JAMA
American Journal
of Public Health
The New England
Journal of Medicine
Number of articles
in a PubMed search
for “racism”
20
10
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
10
20
BRITAIN
30
In a PubMed
search for
“race”
The BMJ
The Lancet
40
50
20
60
10
2013
2015
2017
2019
2021
2013
2015
2017
2019
2021
10
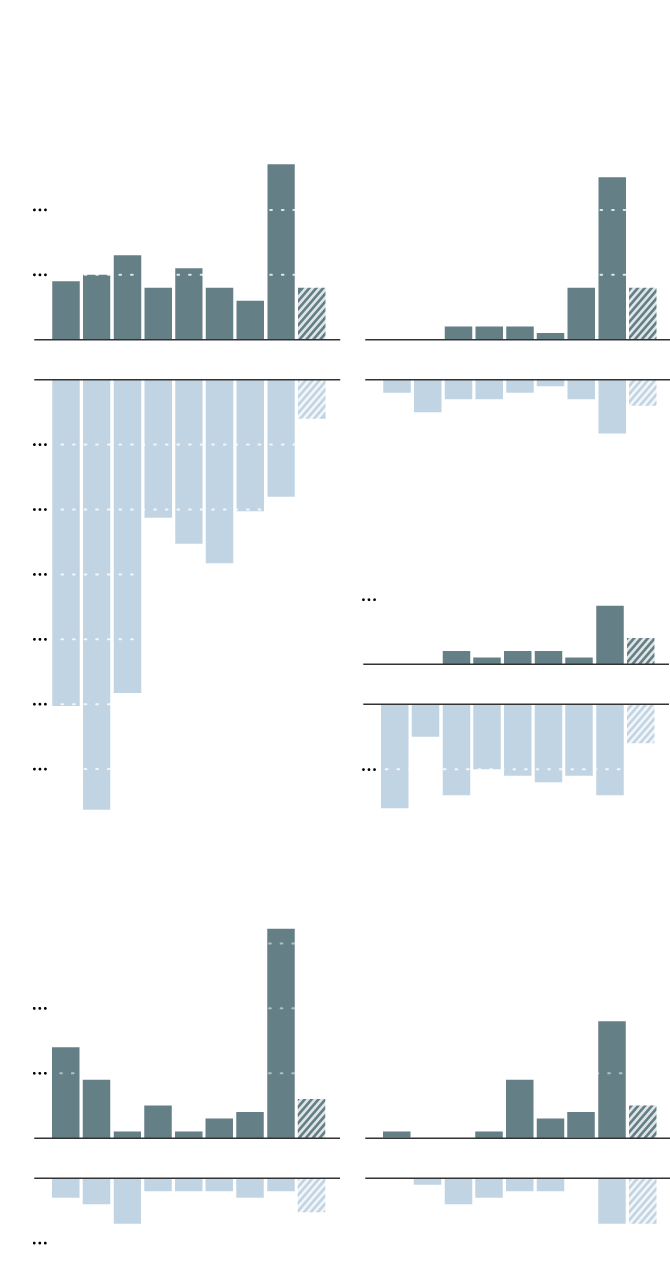
UNITED STATES
American Journal
of Public Health
The New England
Journal of Medicine
Number of articles in
a PubMed search
for “racism”
20
10
2013
’15
’17
’19
2021
2013
’15
’17
’19
2021
10
20
JAMA
30
10
In a search
for “race”
40
2013
’15
’17
’19
2021
50
60
10
BRITAIN
The BMJ
The Lancet
20
10
2013
’15
’17
’19
2021
2013
’15
’17
’19
2021
10
The New England Journal of Medicine rarely addressed racism until the arrival of Dr. Eric Rubin, its current top editor, in 2019. The British Medical Journal and The Lancet, both based in Europe, published more studies on the topic, while the American Journal of Public Health published the most.
At many medical journals, “a lack of scholarship” leads to an approach to health care disparities that skirts any discussion of racism, said Dr. Stella Safo, a Black primary care physician at the Icahn School of Medicine at Mount Sinai in New York.
“Let’s have more editors that have this background, and know how to talk about race and racism responsibly,” she said.
Medical journals like JAMA favor studies linking race or racial inequities to socioeconomic or biological factors, she and other critics said. Less often do their editors, mostly white and male, accept papers that explore how systemic racism shapes the health care experiences of Black and brown people, they said.
JAMA’s reckoning came after Dr. Edward Livingston, an editor in a podcast discussion, suggested “taking racism out of the conversation” about societal inequities and said that “structural racism is an unfortunate term to describe a very real problem.” Communities of color were held back not by racism, he said, but by socioeconomic factors and a lack of opportunity.
Dr. Livingston is white, and the conversation did not include any scientists of color. A tweet promoting the podcast claimed that “no physician is racist,” and was later deleted.
The ensuing uproar prompted Dr. Livingston to resign. The American Medical Association, which oversees the journal, began an investigation.
Following the podcast, Dr. Safo and Dr. Brittani James, a Black physician who practices on the South Side of Chicago, began a petition, now signed by more than 9,000 people, calling on JAMA to restructure its staff and hold a series of town hall conversations with patients who are Black, Indigenous or people of color.
Earlier this month, the association’s leaders admitted to serious missteps and proposed a three-year plan to “dismantle structural racism” within the organization and in medicine.
“I remain profoundly disappointed in myself for the lapses that led to the publishing of the tweet and podcast,” Dr. Howard Bauchner, JAMA’s top editor, said in a statement announcing his departure. “Although I did not write or even see the tweet, or create the podcast, as editor in chief, I am ultimately responsible for them.”

The A.M.A., the largest association of physicians and medical students in the United States, has had a troubling relationship with race. The group apologized only in 2008 for its past exclusion of Black physicians from membership and implicit support of segregationist policies.
“This is a real moment for JAMA and the A.M.A. to recreate themselves from a founding history that was based in segregation and racism to one that is now based on racial equity,” Dr. Safo said.
Other medical societies recently have offered formal apologies for racist pasts, including the American Academy of Pediatrics in September and the American Psychiatric Association in January.
But the A.M.A.’s initiative has been met with opposition from some members, who said in a letter to the organization’s leaders that “there is a general feeling that the firing of the editors involved in the podcast was perhaps precipitous, possibly a blot on free speech and also possibly an example of reverse discrimination.”
“There is no one in health care that has done this right, fully,” said Dr. Aletha Maybank, who leads the A.M.A.’s Center for Health Equity. “We are all making the road as we walk.”
Dr. Maybank was one of four researchers who showed in a recent analysis that even when medical journals address racism, they do so most often in opinion articles, not in evidence-based studies.
In interviews, two researchers described the difficulties in getting their research on racism through the editorial process at JAMA.
Dr. Melissa Simon is director of the Center for Health Equity Information at Northwestern University and a member of the United States Preventive Services Task Force, an expert panel that advises doctors on best practices.
She recalled many unpleasant interactions with JAMA staff, including being talked over on podcasts. “I’m actually glad that they showed their biases to the world, because many of us have experienced these biases with JAMA for a while now,” she said.
Dr. Simon, who is Latina, submitted her research into high death rates among pregnant Black women to JAMA for consideration last summer. Dr. Bauchner cut the word “racism” from the manuscript and watered down the conclusions, she said. After many rounds of revisions, the paper was rejected.
Dr. Simon was flummoxed. “You cannot talk about maternal mortality without racism,” she said. “You just can’t, in the United States of America.”
After editors at JAMA and elsewhere tried to “whitewash” her papers, she said, “I have given up submitting, even trying to submit, manuscripts for potential publication at certain journals.”
Dr. Bassett, who is Black, recalled a very similar experience after submitting to JAMA a paper on the long-reaching impact of historical redlining on preterm birth. In her recollection, Dr. Bauchner excised mentions of racism from the paper and eventually rejected it.
Both papers were eventually published in the American Journal of Public Health.
The A.M.A. declined to comment on the researchers’ experiences or Dr. Bauchner’s departure while its investigation was still underway. JAMA did not respond to requests for comment.
Dr. Bauchner declined several requests for interviews, but said in an email to The Times last month that JAMA had published “more than 100 articles on issues such as social determinants of health, health care disparities, and structural racism over just the last five years.”
He also noted that JAMA accepted only a tiny fraction of the manuscripts it received. Last year the journal had more than 20,000 submissions, and accepted less than 4 percent. Dr. Bassett said she could not rule out the possibility that her papers had been rejected because they did not meet the journal’s standards for quality.
But she noted that JAMA also had rejected her analysis of Covid-19 mortality rates by race and age, while publishing another paper proposing that a racial variation in a cellular receptor for the coronavirus might be an explanation for the pandemic’s disproportionate toll on Black people.
Dr. Simon said “there are gatekeepers along every single step along the path to produce science,” from acceptance into Ph.D. programs and funding for projects, to publication of results and invitation to speak at conferences. Publication in journals like JAMA may dictate which academic researchers get tenure, and which subjects are worth research dollars.
“They have a huge responsibility, because of the power they wield with respect to influencing science,” Dr. Simon said.
Some top journals are staffed almost entirely by white men. At JAMA, for example, 93 percent of the editorial leaders were white, noted Dr. Raymond Givens, a cardiologist at Columbia University in New York.
After JAMA’s podcast, Dr. Givens set about tabulating the race, gender and ethnicity of editors and editorial board members at the JAMA network of journals and the New England Journal of Medicine. The current editor of JAMA Dermatology may be “the only nonwhite editor in the entire history of all those journals,” he said.
Dr. Givens, who is Black, said he did not object to the topic of the controversial podcast. But to discuss whether structural racism exists without having experts on that topic nor Black physicians present was “a complete breakdown of scientific thinking,” he said. “If that’s not structural racism, or even meta-structural racism, I don’t know what is.”
In October, Dr. Givens contacted Dr. Rubin, editor in chief of the New England Journal of Medicine, and Dr. Bauchner, pointing out the disparities in staffing at their journals.
“I note with humor but absolute sincerity that there are more editors named David at your journals than Black and LatinX editors combined or East Asian and South Asian editors separately,” he wrote. Dr. Rubin responded and arranged a meeting to hear more. Dr. Bauchner did not reply, according to Dr. Givens.
“People are just really resistant to the very possibility that somebody might call them a racist, or that we might suggest that they hold racist views or ideas,” Dr. Givens said. “And because of that, there’s this unwillingness, or really this tendency, to shut down the conversation whenever it goes there.”
In an interview, Dr. Rubin acknowledged that the journal’s staff was not diverse enough, but said the low turnover among editors presented challenges to hiring new people.
Since his arrival, the journal has added four editors and four editorial board members, and in June, introduced a section of the journal’s website called Race and Medicine. Although the journal does not have self-reported information on race, half of the new additions are people of color, and three — including the new executive editor — are women, he said.
That’s a step in the right direction, but journals will also have to learn to address racism more directly in order to improve lives, Dr. Bassett said. As health commissioner of New York City from 2014 to 2018, she made confronting racism a central part of her work.
“When you can’t see what’s in front of you, and you can’t talk about it, you obviously can’t solve it,” she said. “That’s just no longer acceptable.”
Advertisement

