As the nation heads further into flu season, it’s unclear whether more shutdowns are likely as people are driven indoors, risking worse spread of the novel coronavirus at a time hospitals are already strained by the flu.
The decision to shut down businesses and gatherings earlier this year may have been a prudent public health decision, but it badly bruised hospitals and providers financially as many recorded steep revenue declines when lucrative elective procedures were halted.
Some health system executives are turning to artificial intelligence and machine learning tools to help them manage electives without the need for more shutdowns.
Leaders at Banner Health, Arizona’s largest provider, argue that volume data from this summer is compelling evidence for why health systems should have the autonomy to direct electives amid infectious outbreaks.
“Rather than ‘I think’, ‘I feel’…we have a tremendous amount of data,” Nirval Patel, medical director of perioperative and procedural services at Banner, said. “That gave us a very objective, consistent reliable framework and we could explain it to others.”
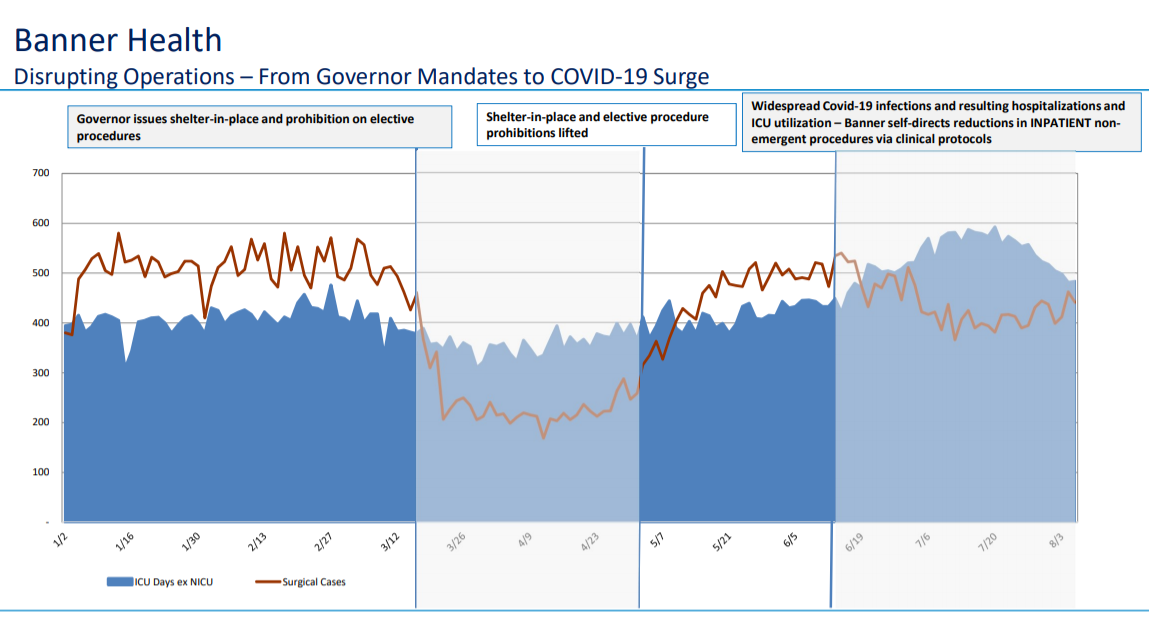
The data show that when COVID-19 infection was widespread in Arizona and hospitalizations reached a peak in June, the system was able to decrease inpatient elective procedures as it faced increased strain from the virus. But the data also show the frequency of surgical cases in June, while lower than during the month prior, was still higher than March and April when under stay-at-home orders.
Harnessing big data
After procedures bottomed out in March and April, Banner decided that once the shelter-in-place orders were lifted it would need to devise a strategy to manage both the strain of COVID-19 cases and to sustain elective procedures, a lucrative line of business for providers.
And by June, Arizona started to see cases of the novel coronavirus surge. It had quickly become one of the nation’s hotspots after Gov. Doug Ducey, a Republican, allowed a sweeping reopening of businesses in May, including bars and restaurants. At one point, the virus was so widespread that officials said contact tracing was no longer effective.
At the peak of Arizona’s surge, Banner said it was managing 50% of COVID-19 inpatients across the state.
Banner commands the No. 1 market share position in a number of key service lines in its flagship state of Arizona, including cardiovascular, oncology and orthopaedics, according to investor presentations.
Executives decided they needed to lean into big data and machine learning to help them navigate the unfolding landscape.
The system, one of the largest nonprofits in the nation, operates 28 hospitals in six states — including two academic medical centers and two children’s hospitals — encompassing more than 5,000 licensed beds.
The decision was to “let our data drive our decisions, not our gut,” Patel said.
Banner formed a global strategy group that was responsible for mapping out a blueprint to leverage its data analytics and turn that into actionable information care teams could use.
What they created was a dashboard that could tell them two important indicators: the complexity of the potential procedure and the resources required.
Ultimately, what they developed was a system to help them make informed decisions about whether to proceed with an elective procedure.
For example, with patients queued up for care, they could ask the system the anticipated length of stay for a certain procedure, potential need for an ICU bed or a ventilator, the level of skilled care needed and personal protective equipment required.
Synthesizing all those factors, the data system could tell the operators where a potential procedure fell in a range from low to high complexity.
The goal was to give surgeons, care teams and patients the confidence to make decisions.
Staff are able to glean from the dashboard that a certain procedure is a low complexity case, if it’s an outpatient procedure and the length of stay is less than one day, and the potential need for ICU is less than 1%, Patel said using an example.
The care teams present this information to patients and let them be a part of the decision making on whether to have the procedure, Patel said.
Nearing capacity signals, the need for shutdowns
Still, some are skeptical of a health system’s ability to manage both COVID-19 patients and electives — at least up until a certain point.
When Arizona hospitals were under shelter-in-place orders and could not perform elective procedures, it was not because the state was experiencing widespread infection. The outbreaks were mainly on the coasts.
But providers across the country were bracing for an onslaught of cases and needed to secure the essential resources such as personal protective equipment, Will Humble, executive director for the Arizona Public Health Association, said, noting the supply chain issues at the time.
Once supply chain issues were resolved, Humble, who previously led Arizona’s Department of Health Services under former Republican Gov. Jan Brewer, said he advocated for the shelter-in-place order to be lifted.
“I did a bunch of advocacy to try to get the governor to rescind that executive order because it no longer made any sense,” Humble, who is also on the board of the Arizona Hospital Association, said.
However, that’s not to say the government should never intervene, he noted.
Once hospitals near capacity and have to start moving patients around to other facilities, that’s when the government should step in and halt elective procedures.
“At that point it makes perfect sense to tell the hospitals you cannot do elective procedures anymore because you don’t want them to turn away COVID patients in their ED because they’re doing elective surgeries upstairs,” Humble said.
If a new administration wins the White House in November, it’s also unclear what appetite it would have for more stringent shutdowns if cases accelerate after inauguration.
Still, these anecdotes from Banner and others give investors and analysts optimism, Ken Gacka, senior director and analytical manger at S&P Global Ratings, said in August during an online webinar on nonprofit hospital performance. He noted that as providers learn more about how best to treat this disease and become more adept at also managing the business side, hard shutdowns are less likely.
“I think the more draconian measures of shutting down electives that we saw in March and April are unlikely to be repeated. I hope that’s the case, too.” Gacka said.
