December 24, 2018
As appropriate initial antifungal therapy has been found to be critical, upfront combination antifungal therapy may be required to increase the probability of survival of patients at risk for invasive
Patients with voriconazole-resistant invasive aspergillosis have a higher mortality rate compared with patients with voriconazole-susceptible invasive aspergillosis, according to study findings published in Clinical Infectious Diseases.
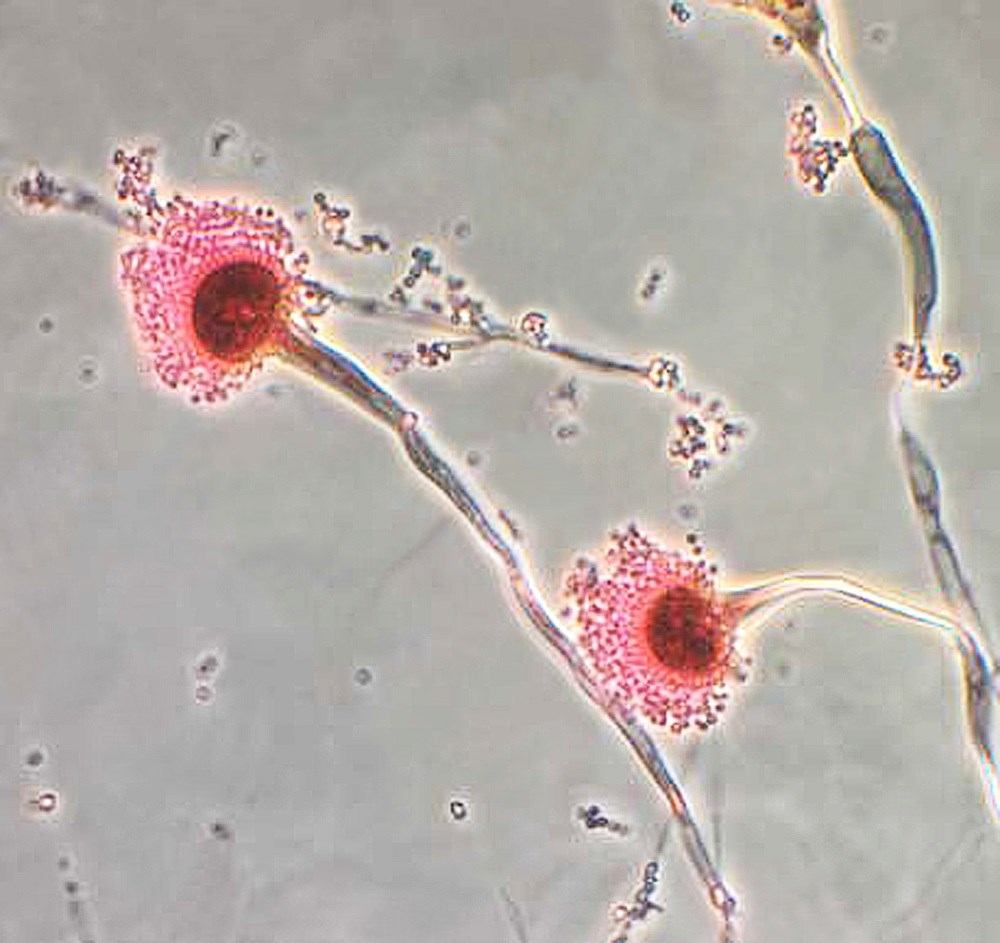
Triazoles are a class of medication widely used to treat invasive aspergillosis, but resistance to these agents has become a concern for managing infections caused by Aspergillus fumigatus. In order to evaluate and compare the characteristics and outcomes of voriconazole-susceptible invasive aspergillosis and voriconazole-resistant invasive aspergillosis, Dutch researchers conducted a 5-year retrospective cohort study that assessed mortality in these two patient groups. Clinical characteristics, mortality at day 42 and 90 after treatment initiation, triazole resistance profiles, and antifungal treatments were evaluated.
The cohort comprised 196 patients from 3 university medical centers who received antifungal treatment within 30 days of a positive culture for A fumigatus. Of this group, 37 (19%) patients harbored a voriconazole-resistant infection. More than half (53%) of patients had an underlying hematologic malignancy and 79% of patients were started on voriconazole. Resistance to voriconazole was associated with a 21% increase in overall mortality on day 42 (49% vs 28%, P =.017) and a 25% increase in mortality on day 90 (62% vs 37%, P =.0038) compared with patients without resistance.
In patients who were not in intensive care, there was a 19% lower survival rate in patients who were voriconazole-resistant at day 42 (P =.045). Inappropriate voriconazole therapy was associated with lower survival at day 42 vs appropriate therapy (76% and 53%, respectively; log-rank test, P =.016).
“As appropriate initial antifungal therapy was found to be critical, upfront combination antifungal therapy may be required to increase the probability of survival of patients at risk for invasive aspergillosis in geographic regions with high resistance rates,” wrote the researchers.
Reference
Lestrade PP, Bentvelsen RG, Schauwvlieghe AFAD, et al. Voriconazole resistance and mortality in invasive aspergillosis: a multicenter retrospective cohort study [published online October 11, 2018]. Clin Infect Dis. doi:10.1093/cid/ciy859
